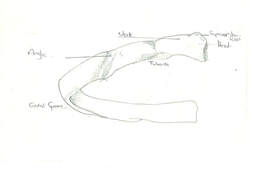
 People ask me what I most often treat. The glib and osteopathic answer is 'people'. If I'm going to be reductionist and nominate a body part then ribs are surprisingly high up there. Why surprising? Well? How often do you think about your ribs? The amount of patients who say 'I have ribs at the back too?' or 'that far up/down'. You break them or bruise them but rib dysfunction with no traumatic onset? I'm being a little disingenuous here, because, most often it is not the rib itself that is the problem but the joint or joints attaching it to the spine and to the sternum (breastbone). Most people have 12 pairs of ribs. 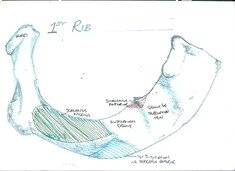 The top pair are the 1st ribs, uniquely they only have one joint at the rear with the spine Ribs 2-7 have two joints at the rear, all of ribs 1-7 are true ribs and have a joint at the front with the breastbone Ribs 8-10 are false ribs, they don't come all the way to the front but join to cartilage which then combines and joins to the 7th rib Ribs 11 and 12 are floating ribs, they only have the two joints to the spine and the front end 'floats' but not very freely as t is held in place by muscles. So what can go wrong? Well the ribs are subject to loads of forces in different directions. Obviously they move when you breathe...you may never have thought of that..and when you move your thoracic spine they have to move to accommodate that and then there are the shoulder movements that basically require your ribcage to deform to accommodate those too. Each time a healthy rib moves all of the joints between it and your spine and sternum should move a little too, but like every other joint, they can get irritated, inflamed, restricted, stuck and the whole rib can end up out of synch with the spine and with the other ribs around it. Which can cause the joints to get very inflamed and painful. and can cause the muscle overlying the rib to be held on stretch for long periods, which then makes the muscle sore and or tight. So many of those 'knots' you get in your upper back between the shoulderblades are not knots at all but instead some muscle stretched over a prominent and unyielding rib below. Then there are the muscles between the ribs, you know, the tasty bit in spare ribs, they are intercostal muscles and can become too tight and feed into the dysfunction by pulling the ribs together unevenly like badly ruched curtains and then there are muscles attaching to the top and bottom ribs, at the top, particularly the scalenes, these are the muscles that run up the side of your neck and they attach to the first and second ribs, poor rib function there can lead to the scalenes becoming tight resulting a stiff and painful neck, not to mention the effect it can have on the nerve and blood supply to the arm. At the other end the 12th rib attaches to quadratus lumborum and psoas, as well as the diaphragm and dysfunction here can lead to low back pain, even hip problems and problems with the nerve supply into the leg. I rarely treat ribs in isolation but, I treat them with most patients and they deserve to have more attention paid to them in general
0 Comments
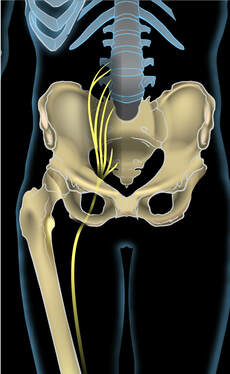 Leg and yes, the gluteal region too. Sciatica is one of those terms thrown around with varying degrees of accuracy, so I thought it might be time to talk about what it is..and isn't...and of course what osteopathy may be able to do to help. The idea behind sciatica is irritation of the sciatic nerve causing pain in the leg. Let's get the annoying 'know it all' stuff out of the way first... 1. There is no sciatic nerve...Really! What we call the sciatic nerve is actually a sheath containing 2 completely separate nerves, the tibial and fibular (or peroneal) nerves. 2. A slipped disc, disc protrusion, herniation etc cannot press on the sciatic (or fibular or tibial) nerve, these nerves are what are called peripheral nerves and are formed outside the spinal column (hence in the peripheral, not central, nervous system). What can get irritated in the spinal column, by a slipped disc etc, is a nerve root. These exit in pairs at each spinal level and then send branches which join in plexuses (plexi?) to form peripheral nerves Phew! OK, so lets assume we are talking about nerve pain, numbness or weakness in the buttock, maybe down the outside or back of the thigh and sometimes into the calf and foot. Where are the main places that the nerve can be irritated? The first place is in the spinal column. A disc bulge can press on the nerve root and cause pain down the leg. Typically L45 or LS discs are particularly prone to herniation and can bulge and press on l5 or S1 nerve roots which cause symptoms in these areas Overtight buttock muscles, especially piriformis can compress the sciatic bundle and irritate the nerves contained within. Typically this is felt as pain along the route of the nerve in the thigh and often doesn't extend beyond the knee although it can go all the way to the foot. The common fibular nerve is prone to injury and entrapment where it winds around the fibular head (the bony lump on the outside just below the knee). Relatively minor knocks here can stop the nerve gliding smoothly meaning that it can get stretched and harder bumps (hit by a car bumper etc) may lead to loss of power from the muscles it supplies, and foot drop. The tibial nerve can get trapped behind the knee, under soleus muscle and in the foot, in a structure called the tarsal tunnel, which can become congested due to poor foot mechanics. How do we know where the problem is? Sometimes it is very obvious from the history, where the injury took place and what kind or injury it was, sometimes examination and basic orthopaedic testing will find an obvious derangement and treatment of that will reduce or eliminate the symptoms. An MRI would be required to confirm a disc bulge and/or nerve conduction testing can show whereabouts a nerve is damaged. Beware though 80% of 40 year olds with no back problems or sciatica will have disc bulges on an MRI. So you may have a disc bulge and sciatica but it may not be the cause, or may be part of the cause and resolving an issue elsewhere may be enough to eliminate the symptoms What can an osteopath do? It depends...as always. If you have herniated a disc, nature may have to take its course, most disc herniations become asymptomatic within 12 weeks (sadly, not all). That said, sometimes even sciatica due to an apparent disc bulge may respond to treatment, either the treatment reduces local muscle spasming, postural issues or fluid congestion around the nerve root thus decreasing compression and irritation, or working elsewhere along the root of the nerve increases it's capacity sufficiently to reduce symptoms. If the problem is due to tight muscles in the buttock we can work to loosen those and, more importantly work out why they have overtightened and work on those factors also. Problems in the foot and further down the leg are often very amenable to osteopathic treatment. Finally, if you are suffering from sciatica it is probably affecting how you sit, walk etc and that will have a knock on effect on other tissues in your back and possibly in your other leg. We can work to minimise those disruptions, so that when your sciatica does go, you aren't left with a whole pile of other problems Picture
Osteopaths treat all sorts of musculoskeletal mechanical disorders and patients seem to come in waves with disorders of particular areas of the body…this week it has been feet.
I have to confess I always approach someone’s feet with trepidation. They aren’t always pleasant and perhaps more importantly they can be tough old things to sort out. We stand on them, and they bear our weight, they’re strong. Similar to the hands I find that I am actually using my hands to make the changes I want, rather than gravity and my bodyweight with other areas of the body, and as a result after treating someone’s feet my hands are usually bright red. As a positive aside I don’t seem to suffer from cold hands as much as I used to before practising osteopathy! So they’re hard work and not always pleasant to work on but feet are so important, for those of us who can stand and walk, they are our foundation and yet we treat them with disdain. When did you last look at your feet to make sure they’re OK? Do they match? Have they changed? Do they move how they should? Patient 1 had a stress-fracture of their 2nd metatarsal for no apparent reason 6 months ago, no bone density problems. It got better and then she started getting pain under the metatarsal heads (the pads just before the toes). When I looked at her foot the medial (inner) arch of the foot was all flattened and the whole foot was twisted so that excessive pressure was being placed on the big toe…and that had responded by developing a valgus (toe bends inwards towards foot at joint) and a bunion, this takes the pressure off the 1st toe and puts it on the 2nd particularly if they have a long 2nd toe, known as a mortons toe…and may explain the fracture. Shockingly the podiatrist prescribed insoles without touching the patient’s feet. The patient was worried their toe had fractured again. I was able to articulate the medial arch to reform but the patient still had pain however we were able to identify it was no longer where the fracture had been, I then worked on the transverse arch, this is the arch across the foot where the pads are just before the toes. Sometimes these can drop and some gentle encouragement can persuade them to pop back into a nice arched shape and voila, no pain. The next step (pun intended) is to see if the foot is capable of holding this improvement without orthotics, and if not, to try with orthotics. Patient 2 had pain in the outside aspect of her left foot, which she had been told was due to an avulsion fracture 2 years ago. On observation the foot had an overly high arch and the toes pulled back almost like a cats claw ready to pounce. She was very hypermobile in her hands and feet, that means her ligaments had much less recoil than usual. She’d been to see a range of practitioners and nobody had questioned this hugely deformed foot, suggesting the pain was just down to a detached bit of bone and she’d have to live with it. Perhaps they thought the foot was like this due to a developmental deformity, it certainly looked like it but I asked the patient about it and the foot hadn’t always been like that, so I decided to see what could be done. Below the talocrural joint there is a joint called the subtalar joint. When we sprain our ankle, it is usually the talocrural joint but can sometimes be the subtalar joint. The subtalar joint was stuck twisting the foot inward and the rest of the mid and forefoot was twisted the other way so the front of the foot could present flat to the ground. After I had released the restricted joints the arch normalised and most of the toes released and sat almost flat, I then massaged the short toe flexor muscles in the arch of the foot and the longer toe flexors and extensors in the leg. The foot straightened out, almost entirely, this crippling condition apparently 90% resolved with 10 minutes work. I think that the patient had just sprained her subtalar joint and in order to protect the hypermobile foot in this less stable position the nervous system had activated both flexors and extensors to hold the foot rigid. Again we need to see how much of the improvement is maintained but even if it starts to revert, this opens new avenues of treatment to explore. The moral of this story is, look at your feet and get problems resolved (including that revolting athletes foot) because feet that function well don’t just help protect against foot and ankle pain but they absorb forces to protect the rest of the leg, the knees, the hips and even the back. Don’t necessarily expect other professionals to identify resolvable biomechanical dysfunctions. Orthopaedic surgeons are primarily looking for things that require surgery, a podiatrist who is an expert in orthotics will probably make you some lovely orthotics. I’m not sure this should be seen as criticism…I’d do a lousy job of removing your bunion and you’ll be pleased to know I wouldn’t dream of trying. “Render unto Caesar…” and all that, there’s a place for podiatry and for surgery but I hope you will now consider that there’s a place for osteopathy in the care of your feet, even if that does mean I have to handle more of the darn things. I’ve written about this before…and I try not to repeat myself…but please forgive me this once as I come to this with fresh information.
I’ve written about how uncomfortable the hard, upright seats on many modern new planes and trains are, notably Thameslink and the new Intercity Express Passenger trains. Im not going to go into why hard upright seats are so uncomfortable again, it's here. It seemed to me that someone was taking perverse glee in commissioning seats that were horribly uncomfortable, except they’re not…any more. I should explain that the seats haven’t changed, my back has! So now I can see both sides of the story. I have spent most of my life with a pronounced kyphosis, that is to say that the top part of my back is more rounded than average. I remember going to an Alexander Technique taster class aged 18 and lying on my back on the floor and finding it painful because my upper back was rounded and hard and wouldn’t lie flat enough to be comfortable. There are many reasons for a pronounced kyphosis, maybe it is genetic, maybe it is the result of having been tall at a time when I was shy and so spent my time looking at the floor, maybe it was the result of falling out of a tree onto my back aged 10 or 11 and the injury not resolving properly, who knows. I have spent the last year and a half working hard on my own body, using self-treatment, treatment from my osteopath, deep tissue massage, swimming, focused gym work and most recently pilates, in order to get mobility into my whole back and then to start to reduce that excessive kyphosis. The good news is it is working and I know that because, my shoulders are less rounded so I can perform lateral raises properly in the gym (I absolutely couldn’t before)…and…wait for it…The seats in the Intercity Express Train are OK, they’re not cosseting but they’re not uncomfortable either. So what does this tell us? Firstly, long-standing postural issues can sometimes be reversed, but it takes a lot of hard work. Secondly, the commissioning team for the latest train seats aren’t necessarily sadists…but they are making the common mistake that catering for the average person is good enough, it isn’t, it is poor design because it is uncomfortable for a very significant proportion of the population. We live in a world where doors and grab rails (rightly) have to be a specified number of shades away from the surrounding colour palette and journeys are punctuated by passenger announcements, to make journeys easier for the visually impaired. Trains are removed from service and stations remodelled at great expense because they aren’t wheelchair accessible. Yesterday at Slough station there were signs all over the stairs on the new bridge and a really annoying announcement every 30 seconds demanding that I use the handrail on the stairs (despite that rendering the middle 2/3 of the staircase potentially useless). Against this backdrop, how can we think it is acceptable to introduce seats without ensuring that they are not cripplingly uncomfortable for the vast number of people in the UK whose back is more curved than average?...and if you are lucky enough to think that this is a moan about a little bit of discomfort, then I hope for your sake your back doesn't lose it's shape and flexibility as you age, because, I can tell you from experience that these seats, so innocuous for most are much more than a little uncomfortable for the kyphotic many. Back down off my soapbox I’d love you all to be able to come and have as much treatment as you need to make your body the very best it can possibly be. Realistically though, many of us (I include myself) have long standing issues that require a long period of sustained and intensive therapy to fully resolve. Apart from the investment in time that can also mount up in terms of cost. Not everyone (I include myself in this also) can afford to commit to open-ended weekly treatment. So what happens is, the patient comes with a problem and if the pre-disposing factors, that is the underlying postural issues are long-standing, complex and slow to resolve then the patient stops coming, once their current pain or dysfunction is resolved…but then they are back 6 months later with the same problem or something else but caused by the underlying issue not being resolved. So how can that be minimised? Over to you, the patient, to take some control of the issue
 I’ve just been on a course that challenged my thinking about how joints move. We were asked to think about how many ways a spinal joint can move. Classic thinking is that it can flex (bend forward), extend (bend backwards) side bend left, and right and rotate left, and right. Thinking a little harder and the joint can also translate, that is traction or compression can be applied and obviously it can have varying combinations of the above. But, in order to achieve left rotation at the C3-4 joint, that is C3 vertebra rotating left relative to C4 vertebra there are 5 different things that could be happening C3 could be rotating left on a fixed C4 C4 could be rotating right under a fixed C3 C3 could be rotating left and C4 could be rotating right C3 and C4 could both be rotating left but C3 is moving faster, and C3 and C4 could both be rotating right but C3 is moving more slowly That works for all of the directions of motion. Why is that important, beyond an interesting brain teaser? Firstly it can give us more information. If C3 won’t easily rotate left on C4 but C4 will rotate right on C3, perhaps the problem isn’t with C3-4 but instead C3 cannot rotate right under C2 Secondly, it gives more treatment options. If you can’t turn your head to the left without pain, perhaps, instead you can fix your stare on a point and reach forward with your left arm, rotating your shoulder girdle to the right. That is still rotating the top part of your neck to the left relative to the bottom part but is coming at it bottom up, rather than top down. This can be incredibly powerful and can be applied in all ranges of motion throughout the spine  Knots are part of the massage lexicon, they are little swollen, hard tender bits of muscle and are thought to occur when there is injury, possibly in response to increased calcium in the area causing localised bunching of muscle fibres with an inflammatory response. Except sometimes... It's a rib! - ribs 2-10 start at the spine and wrap around to form your ribcage before joining your sternum at the front. These ribs start out pointing backwards and to the side and then after approximately an inch there is a sharpish corner, after which they point to the side and even a little forward. This corner is called a rib angle and at this point the rib has a joint with the transverse process of the vertebra. If the vertebra is twisted to one side then that costotransverse joint will be prominent on that side, or if the joint isn't functioning properly the rib may sit a little out of line, or indeed there may be inflammation that can be palpated, all of these will feel like a 'knot' between the spine and the shoulder blade and they will be covered with muscle that may be sore, because it is being permanently stretched over a lump. When it's an inflamed facet joint! In the neck, the little joints on the back of the spine can be felt...and when they are inflammed the soft tissues of the joint swell...and make a lump...that feels like a knot All in all, whilst knots may appear over joints, the chances are that if there is a lump localised over a joint it is related to that rather than the overlying muscle. working on the muscle over the joint may release the joint and resolve the issue but...the issue was not a knot!  I hate this question...but completely understand why patients ask me...and do my very best to answer it honestly...or as honestly as I can. It goes with "is it better this week?" in the category of difficult questions. As an osteopath I satisfice, that is to say I am not looking for perfection, I am looking to do enough to allow you to get back to normal activity with no, or minimal pain. I do that by finding dysfunction and working to resolve it...Or do I? To the osteopath your body isn't made up of discrete structures, joints, muscles etc which can be checked for dysfunction, repaired and ticked off, that would be lovely but that was of looking at things is completely at odds with the core principles of osteopathy. Firstly, one of the principles states that "the body is capable of self-regulation, self-healing and health maintenance", or alternatively "the body is its own medicine cabinet". Now don't get me wrong,I don't believe that we understand how to unlock the body's potential to heal all insults and indeed I doubt that is possible but, I do believe that the treatment I give, is not really the cure, it is, merely removing impediments to the body curing itself. Realistically, sometimes that is as near a cure as makes no odds. If a structure is being held awkwardly and a technique releases it then to all intents and purposes it is a cure, but more often the process takes time and there are stages by which treatment allows more normal movement and then that normality of movement improves tissue health and in turn allows treatment to further increase normality of movement. This change occurs on many levels:
So, when someone asks whether it is better than last week, the only person who can answer that is them..really. I can point to improvements in movement and in tissue tone and texture, but only they can tell me whether they are nearer to achieving their goals and indeed, only they can identify those goals in the first place. How many sessions you need depends on your goals, your starting point, and how you respond to treatment, mentally as well as physically...as well as effective treatment of appropriate tissues. As a rule of thumb, I expect to see significant improvement by 3 treatments (often sooner) but everyone is different, long-standing problems often take more treatment, often the patient gets a lot of benefit from the first few treatments but then the additional benefit from each treatment tapers off...but not always...and sometimes there are additional breakthroughs where significant improvement occurs after a period of relative plateau. The important thing is communication, I need to understand whether you are feeling benefit and I need to be honest about my best assessment of what can be achieved in the short and medium term and that puts you in control, of what you allow to be done to your body and how much time and money you are prepared to spend.  The most important job we do is screening for serious conditions that require referral. Much of our training revolves around the identification of serious pathologies and the case history, even more than the examination, is designed to spot them. So, what clues are we looking for? We are looking for: Onset - Was there a trauma, that makes a mechanical, musculoskeletal injury more likely, of course, if the trauma is severe, the patient may have fractures which are a contraindication to treatment, so judgement is still required Progression - are the symptoms worsening for no apparent reason? Location - Musculoskeletal problems don't tend to occur simultaneously in multiple places Comorbidities - Are there other siulatneous symptoms which could suggest infection, neoplasm or another systemic disease process Aggravating and relieving factors - most musculoskeletal pain is aggravated and relieved by position and/or movement. Inflammatory pain is helped by anti-inflammatory drugs Nature and site of pain - Is there a musculoskeletal structure which causes pain in the right place and with the right characteristics? It is with this in mind that I was presented with a 75 year old woman who spoke no English and whose daughter translated for her. She looked very unhappy and actually cried as she described her symptoms. She had pain in both arms and shoulders of two months duration, which was worst on waking and was progressing. She felt her grip was reduced and she couldn't raise her arms above the horizontal. She also described pain in b hips and down legs to feet. She was advised by the GP to have and x ray which showed some wear and tear in the neck. At this point I am thinking 'no way is this musculoskeletal' and I am wondering whether I should stop her there and send her for blood tests for, amongst other things, polymyalgia rheumatica (PMR), a not uncommon condition affecting mainly women over 50 and affecting the hip and shoulder girdles. We continue with the case history and it emerges that she had a fall a couple of months prior to the symptoms commencing, landing on her left outstretched hand, but was fine after a little physio. Critically the patient wasn't getting any headaches or visual disturbance (more of that later). Upon examination the woman was very kyphotic and the shoulders were very protracted, her upper rib cage was hard and unyielding and some of the ribs were prominent and causing the shoulder blades to tip forward. I explained that the onset of symptoms in multiple places suggested that there might be something systemic behind this and that blood tests might be required but that I would be happy to try a gentle treatment, if she was, to see if there was a musculoskeletal element. Crucially the lack of headaches made it very unlikely that, if the condition was PMR it was not yet accompanied by its dangerous bedfellow giant cell arteritis (GCA), which can cause blindness, and so urgent further investigation was not required. I treated the patient using articulation techniques to get the upper back and ribs moving, bearing in mind that the patient was very kyphotic and of an age where I needed to treat her as though where she may have osteoporosis . This week I saw her again and she was all smiles. The left arm still hurts in some positions but she can raise both arms and feels her grip is returning, the right arm feels almost back to normal...and the legs? I don't know if it was mistranslation or just exaggeration born out of fear and pain, but it appears that the problems in the legs are just around the knees and are caused by varicose veins and that there is no problem in the hips. I haven't ruled out something systemic, all diagnoses are provisional, but it looks like this was a case of a mechanical problem masquerading as something more serious. I'm glad I took the chance to treat and see.  I'm not talking about the old word for homosexuality. I'm talking about your ankles. So what does inversion mean in respect of you ankle? Technically inversion is a movement in one plane only, meaning sidebent inwards . In reality, most of the time we are taking about about supination, which is a movement in 3 planes of motion, if you know your anatomical terms then it is made up of inversion of the hindfoot, adduction of the forefoot, and plantarflexion of the talocrural (ankle) regions. If not, don't worry just think that inversion is a pure movement at one joint in the heel and supination is the more complex movement that occurs more often in reality. Your foot tips into inversion/supination much more easily than it does into eversion/pronation...try it, it turns inwards easily and a lot and outwards not so much. As a result most ankle sprains and twists are into inversion. I have been surprised how many of my patients presenting with all sorts of issues have one or two ankles which are held in inversion, that is to say that either the hindpart or the whole of the foot can't present straight to the floor. How can this occur? Well, you can have a pure supination, it can occur in the talo-crural joint (talus top bone of foot and and crus, referring to the paired leg bones) where the tenon like talus gets wedged supinated betweeen the two sides of the mortice formed of the ends of the tibia and fibula, or the sub talar joint can become restricted and hold the foot in the inverted position. In addition the tibialis anterior and posterior muscles in the shin and calf can become tight or shortened and contribute to holding the foot in this position and I have often seen a fixed twist in the midfoot as it everts to reverse the deformity and present the forefoot flat on the floor. Without correction this fixed twist will also be acting to maintain the inversion of the back of the foot. Finally, right up by the knee is you superior tibiofibular joint, if that gets stuck in a position with the fibular relatively inferior to its proper position then the whole mortise of the talocrural joint will force inversion How do I spot this? It's very simple. When I look at you from behind, your achilles tendon should run in a fairly straight line and the bulge of your heel bone (calcaneus) should be approximately symmetrical either side, if not, something is wrong. I can confirm this by feel and by feeling whether it moves evenly compared to the other side and the range of normals I have felt over the years. If the heel has been like this for some time the insertion of the achillles tendon will even move so that it no longer attaches at the pointy top of the calcaneus but instead attaches to the side, I can feel this too. Why is this important? Well, the first effect will be on your foot. If your hindfoot is pronated you will need to twist through your midfoot to place the front of the foot flat when you walk and that may cause problems in the midfoot and tightness in muscles which are being over-stretched in the shin, maybe even shinsplints. You may not have the midfoot mobility to do that so may be walking on the outside of your foot...or more likely as you present your foot flat your knee has to drop inwards (valgus) to compensate. Therein lies a whole can of worms. When you have a knee valgus, first of all you are going to be stretching and stressing the ligament on the medial part of the knee (the inner part, nearest your other knee). The medial collateral ligament, as it is called, is attached to the medial meniscus, this is a cup shaped piece of cartilage which sits between your femur (thighbone) and your tibia (shinbone). If you are stretching the medial collateral ligament you are also deforming the medial meniscus and may well make it more prone to tearing. what is more the proportion of the weight taken by the lateral meniscus has increased, making that more prone to damage also Once a structure is out of line, as with a knee in valgus then it is not supported against gravity by the structures beneath it, to stop it collapsing force is required, this is supplied by muscles. Locally, vastus medialis oblique (VMO) is the muscle that tries to stop it dropping. Over time over use of VMO can lead to it becoming over tight or fatigued and ineffectual. As one of the quadriceps muscles it contributes to the joint quadriceps tendon which encapsulates the kneecap, imbalances in the forces inputting into this tendon can cause the knee cap to become bound down onto the structures below or to move in an irregular fashion (maltracking), both of which can cause pain, damage to the cartilage on the back of the kneecap, and eventually arthritis. Your body also stops the knee dropping further inward by pulling the hip outward, using gluteus medius and minimus. Gluteus maximus and tensor fascia lata are also involved as, via the iliotibial band, they try to hold the knee joint close and stable. All of these muscles can become over tight or fatigued as a result of this process and iliotibial band tightness can occur, possibly leading to trochanteric bursitis. Of course, most of us don't have symptoms, but what damage is this storing up for the future. Is this a significant contributing factor for knee, or even hip osteoarthritis? I don't have any evidence to say it is, but mechanically it seems reasonable to assume that there will be long-term effects. I also wonder how many people get a running shoe based on how they weight bear but are actually not weightbearing as they should...and most of the time this is so easy to fix. Anyway, next time you see someone from behind with flipflops on, or bare feet, take a look, you'll be surprised how many inverted ankles you'll find |
Archives
February 2024
AuthorDamian is the principal osteopath at Vauxhall Village Osteopathy and Oval Osteopathy Categories
All
|

 RSS Feed
RSS Feed


