|
So how do we justify our approach as cost effective?
a drug may contain multiple ingredients and testing those ingredients in isolation may not give you many clues regarding the drug's effectiveness, moreover, if the drug has been designed specifically for that patient, it may not tell you how well that combination will work for another patient, in addition there is the placebo effect Is it time to recognise that the placebo as a reference against which to measure non-chemical interventions is nonsense? When we try and break down a complex and unique intervention into individual elements so that they can be tested against someone having ostensibly a similar experience minus that intervention that becomes so artificial it is pseudoscience and importantly disregards the nature of osteopathy. Osteopathy is not defined by 'cracking' joints or by craniosacral therapy or by any particular technique. It is not the same thing to everyone...which makes things very difficult...but it is not about the techniques used, at least not at a granular level. Without looking up the latest agreed definition (which probably comes from the US where they do both more..and less... as osteopaths than the UK tradition) I would say that at its heart osteopathy is about using non-pharmaceutical techniques to treat people with dysfunctions that are largely (but not exclusively) musculoskeletal. A T Still the originator of osteopathy created it in response to the deaths of three of his children from meninigitis and saw it as a full system of medicine in opposition to the brutal heroic medicine practiced at the time and believed that a body free of osteopathic lesions would be a body that could resist disease in all its forms. There are many possible applications for osteopathy and the boundaries of what it is appropriate to say we treat are contentious...so lets start with the basics...musculoskeletal issues. Whilst I said that osteopathy is not the sum of the techniques used I think it is useful to think about they might constitute:
I want to separate out pharmaceutical intervention. It doesn't form much of UK practice whereas it is almost ubiquitous in the US. It is not part of the uniqueness of osteopathy even if at some time it would be useful to understand how effective co-treatment could be. Cranial osteopaths and those who use lots of manipulations are almost mutually exclusive, both eyeing the other with a degree of suspicion and in the middle there are osteopaths who may use little or none of either and can sometimes be quite sniffy about both Where I am heading with this is that it would be useful to classify osteopaths into different cohorts, in order to assess their effectiveness for patients with particular and that perhaps the faultlines broadly fall into three categories
Then, part two, we need to work out what they are treating, and in this we should avoid over medicalisation. Luckily this is already happening. Diagaoses such as non-specific low back pain are more honest than trying to pin the cause on a particular structure or tissue, at least when there has been no trauma Thirdly there are different cohorts of patients, do we split them by age, lifestyle factors, health beliefs, chronicity, co-morbitities etc It's a pretty complicated matrix but in my opinion if we want to truly test how effective an osteopathic approach to treatment is then that is what we need to work towards , in the meantime my fear is that a less granular approach risks throwing the baby out with the bathwater and that would be a terrible shame...and not evidence based medicine
0 Comments
Osteopathy, when performed at least moderately competently is reactive, not prescriptive. The osteopath is constantly monitoring the structure, the tissue on whch they are working feeling for a return to normality, or the sense that no further change will be forthcoming, the technique, used by the practitioner to achieve the change may well be constantly changing fractionally in response to the perceived needs of the patient's body.
Moreover osteopathy tends to treat very widely, both physically, 'the knee may have a strain of the medial collateral ligament but is that because there is a problem with foot and ankle mechanics and that is causing a gait pattern thatcauses that or is preventing it from healing...is that also then causing an assymetry in the back which may be leading to other problems?'...and beyond, 'is this patient cycling and reinforcing this bad pattern, have they recently split up with their partner and sleeping on the sofa and the poor sleep is affecting their recovery?' (note I am not saying we do the work of counsellors but we do provide a listening ear). This creates a problem. How do we measure the effectiveness of interventions so that we can compare and understand what works and what doesn't? Our interventions are complex and multifaceted. What is the active ingredient in osteopathy and what is placebo? How do we determine which part of our treatment is effective and which part is a waste of our time and the patient's, insurance company or NHS's money? It is made all the more complicated by the fact that osteopathy is a broad church. There are some osteopaths who only use very gentle techniques such as functional techiques and cranial osteopathy, others including me prefer, where it is safe to put some force through a joint or work on it persistantly until it starts moving. I've had effective treatments from both modalities but I've also had patients who have had multiple 'gentle' treatments to no effect and have improved massively from one treatment using more direct techniques. Is that down to the previous osteopath's personal competence, the general effectveness of those 'gentle' techniques or just a mismatch between that patient's need and the type of treatment they got...That may include some element of 'placebo' as they felt like I was doing something, whereas they were not convinced the other treatment did. (I do treat more gently when the patient doesn't want or isn't appropriate for a direct approach...and sometimes refer when I tihnk they would be better suited elsewhere). So how do we measure osteopathy? More on that next time Every now and then a patient comes in and when I ask what they want from treatment they answer some variant of "I've got bad posture" "I've got a hump" "fix my text neck" etc, or worse, "I've seen this video online, where they take this boy and straighten him out". I am going to confess now. I think I came to osteopathy based on a false belief. The mother of a boy in my year at school, who lived in the same road as me, walked with a terrible stoop and one day that stoop was gone. I think I asked my mother what had happened and my Mum said thought she had been to the osteopath. I was impressed...but with hindsight, I think my Mum was guessing (they weren't particularly friends). I suspect she had surgery and a rod put in to correct a very severe kyphosis. The thing is that a deformity (I tried to think of another word, but this was an extreme variation from the norm and will have drastically affected her quality of life) like that held for years will have changed the shape of the structures - caused the vertebrae to become wedge shaped, shortened muscles ligaments etc at the front and lengthened them at the back - even if the initial injury was reversable at the time. That is why the surgery is not just a release but a rod is needed to hold the back in position.
By the same token, even if we can release tight tissues, stuck joints etc holding something in a sub-optimal position without surgery, the stretched ligaments and lengthened muscles on the outside of the curve aren't going to ping back with magical elasticity. Something that has built up over years will take time and concerted effort to correct and indeed it may only be reasonable to manage it rather than completely reverse it. If this all sounds very negative, it isn't! We can usually correct things that have happened recently and we can often improve older injuries to improve function and reduce pain. Osteopathy can also play a part in significant postural change but as a part of a wider program, over time. I keep banging on about Pilates because it helps you to strengthen your postural muscles, including reinvigorating tone that has been lost by being stretched over time. I am still slowly correcting my own assymetries and imbalances, using osteopathy to periodically release tightened and stuck tissues and joints and to integrate change, as well as Pilates, swimming and strength training to build new tone Oh and by the way, if you've seen those videos, no I don't do the osteopathy with a plank and hammer, or one yank on a chin strap I'm a great believer that regular exercise and movement will mean fewer visits to the osteopath. Not only will you suffer fewer injuries but they are likely to resolve more easily.
One of my favourite ways of achieving this is Pilates. What I especially like about Pilates is that a good class will see you stretching most parts of your body and conditioning many of the smaller postural muscles as well as the abdominal core. It is also very adaptable with classes available at all levels and your teacher can also give you variations on exercises to suit your own abilities and stage of development. I also enjoy the classes The Pilates method was developed by a German, Joseph Pilates, during the first half of the 20th century, initially whilst interred at Knockaloe internment camp during the first world war, where he practiced his ideas with his fellow internees. As well as mat work, often using small apparatus such as rings, balls, bands and rollers Joseph Pilates also developed a range of apparatus designed to accelerate the process of stretching and strenghtening. The most popular of these is the Reformer...but there are a range of others, including the Cadilllac...which really does look like an instrument of torture! Pilates's father was a gymnast and I think this shows in the practice that now bears his name. There is more similarity than difference with yoga...but the emphasis is more directed to core strength and there is no spiritual element....although it can be quite meditative. Pilates wanted his method to feel like a workout and I have been to some classes that burned like leg day with an evil PT at the gym...but not all classes are the same. The accepted description for Pilates is "a mind-body exercise that requires core stability, strength and flexibility, and attention to muscle control, posture and breathing", that's quite a remit and different classes and instructors will have different areas of emphasis. I thought it might be useful to talk about the different classes I have attended, so that you can get an idea about what is on offer and what might be suitable for you. I am lucky in that my Vauxhall practice is situated in Embody Wellness and I can organise my patients so that I can attend a couple of classes a week, sometimes three. All of the classes at Embody Wellness are mat based, although they do have a reformer available for 1-1 sessions. I started out with bodycare pilates, which is taught by John Hobbs and fits nicely with the days I work at Embody Wellness, being Tuesday and Thursday at 10:00 (he also does level 1-2 pilates on other days which is similar). This class is aimed at anyone and has attendees in their 70s and 80s as well as beginners and those who just want a class that is about maintaining movement and flexibility and is perhaps less focused on strength. There is not a great deal of standing work in this class although there is usually a balance, most of the work is lying down either on the mat or using the equipment to enhance the stretch or provide a balance challenge during strength work. John likes to use all of the small equipment and we usually start with quite a pile of bits and bobs beside us. If you haven't done pilates before I would suggest something like this or some 1-1 sessions before joining a more advanced class. Just because I have said it is lying down doesn't make this a rest. I struggled to start with but picked it up pretty quickly. Suzie Lovelock teaches at Saturday lunchtime and I have challenged myself by attending her 'dynamic pilates' class on a number of occassions. This is of a completely different order of difficulty. This is where I really feel the burn, usually in my legs and glutes. Lots more standing work, poses held for longer, more demands on core strength. This class makes me sweat, and stumble, and exposes my weaknesses both in terms of coordination and strength. Just because I could leg press half a metric ton didn't mean I could hold a lunge whilst rotating and moving my arms! This class has changed title to 'strength and flexibility', when I get the chance I look forward to seeing what's changed. Kelly Balmer also teaches strength and flexibility and I have started swapping my Tuesday class to this. The level is pitched somewhere between the other two. Kelly's class possibly focuses on core strength most of the three and Kelly is all about form. I'll be honest here. I can't do a proper roll-up or roll-down yet (like a situp but a controlled movement spinal segment by spinal segment) but I'm enjoying gradually getting better. If this reads like an advert for Embody Wellness please know I get a staff discount of 20% but do pay for classes and am not paid commission or to promote them. I am writing this because I genuinely think Pilates is an excellent adjunct to osteopathy in maintaining body function. That said I going to give them one last plug because they do offer a discount rate of £45 for your first 5 classes, click here. I hope to see you there. I was flicking through old articles and I came across this one, suggesting that we were not far off finding ways to slow down, pause, or even reverse some of the significant processes of ageing. The article is looking at ageing at a cellular level and is from the perspective of a biologist who is looking drugs that reduce the cellular effects of ageing. Don't get me wrong. I am excited by that but it is only half of the equation. We have it in our hands to do the best with what we've got . Three of the four key osteopathic principles are valid here.
So many people are working from home right now and, if we are to believe what we are told, it will be the new normal for many, at least part-time. In some ways, that is great. Most people won't miss the commute and in theory, at least, that is time you can repurpose to do what you want...and apparently cosmetic and deodorant sales are down, so that suggests you are repurposing some of that wash and brush-up time too. The down side is that for most of us, at least here in London, space is at a premium...we don't have a room set up as an office...so we have to work in our living space and that might involve some compromises. How can you make that work?
Coronovirus, what can you do?
I don’t propose to repeat the advice you are getting elsewhere but I do think there are a couple of points from the osteopathic perspective that bear consideration If you have a mild dose of Coronovirus and can potter around, do so, your body relies on movement to maximise the efficacy of your immune system but the important caveat here is, without exhausting yourself, remember you are not replenishing your oxygen as efficiently so don’t use up everything you’ve got What can you do before widespread infection hits? Try and get your rib cage working as well as possible. Fibrosis will restrict your lung capacity so you want to get your thoracic capacity as good as possible beforehand and make breathing as easy as possible (if you are asthmatic or have other longstanding lung conditions speak to your GP before doing anything that affects your lungs). I suggest yoga or pilates for movement or just some daily stretches at home, open book, cat camel , or an exercise that makes you take deep breaths like running (try couch to 5k) this will also improve your stamina, which is the ability of your blood to carry oxygen. MORE THAN ANYTHING ELSE WASH YOUR HANDS THOROUGHLY AND REGULARLY AND STAY HOME IF YOU ARE AT ALL UNWELL! It’s January and many of us have made promises to shift the Xmas pounds (maybe from more than one Xmas!). I am coming round to the idea of ‘couch to 5k’. I haven’t run yet, but I’m thinking about it albeit still on the couch.
For those of you who are taking up running this January, I have a few thoughts for you to try and help you do it without injury.
 Some of you may have been to multiple osteopaths and may have been surprised by how different your treatment has been. It would be fair to say that osteopathy is a broad church! If you had asked me, before I trained as an osteopath, what defined osteopaths I would probably have said, the type of treatment they offer and would probably have said specifically the use of high velocity thrusts, or, manipulations…because that was the kind of treatment I had from the osteopaths I had visited and I felt that was what was different from massage or physiotherapy. But there are plenty of osteopaths who don’t use manipulations and, of course, Chiropractors use ‘adjustments’, which amount to the same thing…in fact they have probably been using them longer. What makes an osteopath, is more about how we think than any individual technique, or protocol and it is the philosophy that sets us apart from chiropractors, physiotherapists and other bodyworkers. There are 4 key principles of osteopathy
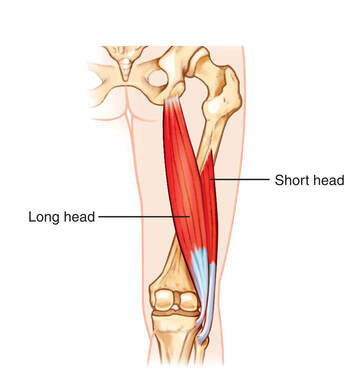 During the first year of training to be an osteopath I spent a lot of time learning anatomy from textbooks. These books describe structures and tell you the names, locations, relations (what is around it), blood supply and nervous supply, amongst other useful information and we (try to) learn these by rote so we can pass our anatomy exams. Some time later…it was the third year of training for me…I suddenly realised that I could differentiate between two structures at different depths by reference to my anatomical knowledge and comparing the shape and, particularly in the case of muscles, lines of force. My particular road to Damascus moment occurred when I felt something pulling up towards the neck from the angle of the scapula (part of the shoulderblade). The trapezius muscle is the most superficial muscle here but I realised the fibres don’t run in that direction, whereas underneath it is levator scapulae and this line of tightness corresponded exactly with where that muscle should run. Over time I became more and more able to differentiate between different structures using this method and I rarely think about the textbook anatomy. Today a patient came in with a pain in his buttock (we joked that I should entitle this, ‘the pain in the bum patient’). On examination the tender bit was in the lower part of gluteus maximus, just above the ischial tuberosity (sitting or sitz bone) but the area affected didn’t run in the same direction as the fibres of that muscle, nor indeed the small internal rotator muscles that lie underneath (and provoking those muscles didn’t recreate the pain), it was also a bit too high to be ischiogluteal bursitis. I was stymied for a moment…and then I remembered that I had read a paper highlighting that a significant minority of people had an anatomical variation whereby their biceps femoris (the outer hamstring) either additionally or often alternatively attached to the transverse ligaments of the sacroiliac joint rather than the ischial tuberosity and realised that this explained the symptoms in this location. There are many anatomical variations, extra ribs at the top or bottom of the ribcage, extra or fewer vertebrae (actually just more or less of them that are not fused; kidneys and nipples often appear in greater number than is standard and sesamoid bones are non-standard parts in more than one place in the body. Understanding how ‘the body’ works is a wonderful thing, understanding how the body underneath my hands is put together is even more exciting |
Archives
February 2024
AuthorDamian is the principal osteopath at Vauxhall Village Osteopathy and Oval Osteopathy Categories
All
|

 RSS Feed
RSS Feed


